Former medical director for insurance giant Aetna in California has admitted under oath that white people are routinely denied healthcare in California because of their race.
Medical director Dr. Jay Iinuma said the task of approving or denying care was delegated to nursing staff, who would “routinely deny whites healthcare coverage while approving those for blacks.”
According to current and former employees of Aetna in California, whites in California are four times more likely to have their claims with Aetna denied than blacks.

BYPASS THE CENSORS
Sign up to get unfiltered news delivered straight to your inbox.
You can unsubscribe any time. By subscribing you agree to our Terms of Use
California Insurance Commissioner Dave Jones expressed outrage after receiving a copy of the Dr. Iinuma’s testimony and said his office is looking into how widespread the practice is within Aetna. According to Jones:
“If the health insurer is making decisions to deny coverage without a physician actually ever reviewing medical records, that’s of significant concern to me as insurance commissioner in California and potentially a violation of law.”
Aetna, the nation’s third-largest insurance provider with over 23 million customers, claims it looked forward to “explaining (their) clinical review process” to the commissioner. However, current and former staff at the insurance giant describe a purely arbitrary claim process in California, riddled with institutionalized racism against whites.
A former staff nurse, who regularly handled claims, said on condition of anonymity:
“I mean there were thousands and thousands of claims a day that each one of us had to handle, there was just simply no way that anyone could run through that much detail. So I just figured if you’re black or Latino, chances are, you need all the help you can get.”
“We even had a saying at the office, ‘If they’re black, have their back, if they’re white, they’ll be alright.‘”
RSJ reports: According to Iinuma’s testimony, he claimed to have been following Aetna’s training, in which nurses reviewed records and made recommendations to him. Jones said his expectation would be “that physicians would be reviewing treatment authorization requests,” and that it’s troubling that “during the entire course of time he was employed at Aetna, he never once looked at patients’ medical records himself.”
One such white patient who needed help but slipped through the cracks was 23-year-old Gillen Washington. Washington, a college senior who suffers from a rare immune disorder, was repeatedly denied coverage for an infusion of intravenous immunoglobulin (IVIG) when he was 19. He is now suing Aetna and alleging the company’s “reckless withholding of benefits almost killed him.”

Washington’s pre-authorization denial of care was signed by Iinuma, who admitted that he had never read Washington’s medical records and that he knew nothing of his disorder. Instead, Iinuma had based his denial entirely on a nurse’s recommendation. It is unclear if Washington’s denial of care was racially motivated.
But Washington’s case is not an isolated one.

Cara Pressman, a bubbly 15-year-old white girl who has suffered from seizures since she was 9 was denied a minimally invasive brain surgery that could have cured her of her seizures and allowed her to lead a normal life. When the seizures strike, her body gets cold and shakes and she completely zones out for between 20 seconds and two minutes. The surgery could have saved her a life plagued with seizures, but her claim was denied by Aetna.
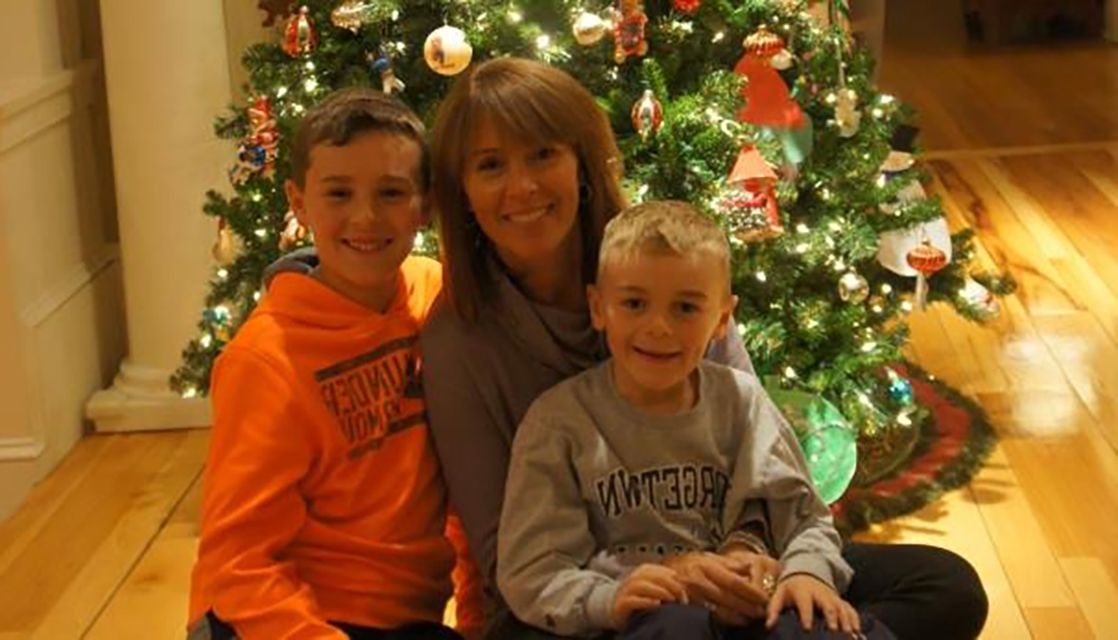
Jennifer Rittereiser, a 44-year-old white mother-of-two was also denied laser ablation surgery by Aetna for her debilitating seizures. Rittereiser said,
“I just want to stop having seizures so I can spend more quality time with my sons.”
Because of the seizures, which can happen at any time, Rittereiser is unable to drive anymore. Last April, Rittereiser lost consciousness behind the wheel of her silver SUV while driving with her 7-year-old son, Robert. Her SUV rammed into a car in front of her and struck it again before veering into oncoming traffic. Her vehicle careened down an embankment, flipped over and came to rest on its side amid a tangle of brush. She narrowly missed slamming into a guardrail and several trees. Somehow both mother and child were able to free themselves and walk out of the SUV unharmed, but she swore never to drive again after that.

Washington, Pressman and Rittereiser are just the tip of the iceberg when it comes to systemic racism and denying the insurance claims of white people. According to a former claims executive at Aetna, who is white and who spoke on condition of anonymity:
“You’d like to think that there’s a team of medical professionals who are sitting down at a conference room somewhere and pouring over your medical records and you claims before deciding whether or not to approve your procedures – but that’s just fiction.”
“It can be based on something as arbitrary as the neighborhood you live in. Like if I know that you live in a rich, white, neighborhood, I would routinely deny your claim – you can afford to pay out of pocket yourself, but if you lived in a poor black neighborhood, I might ‘feel’ for your situation and just let yours through.”
“There aren’t enough doctors to go around studying every case file that comes in.”
The opacity of Aetna’s claim process and limited avenues for appeal, with their arbitrary outcomes, has led to systemic abuse at the insurance giant. On a whole, current and former employees allege that, without considering the seriousness of the medical condition of the claimant, whites were four times more likely to have their claims with Aetna denied than blacks. The lawsuit brought by Washington may be just the first inning for Aetna, which may have to contend with allegations of racism and bias in its claims handling procedure. According to a former employee at the insurer,
“People are running their own little fiefdoms over there. It’s chaos. Anyone can approve or deny a claim, it’s more who you know, whether the nurse is racist. It could be anything.”